Created by Section 3021 of the Affordable Care Act (ACA), the Centers for Medicare and Medicaid Innovation (CMMI; aka The CMS Innovation Center) has been tasked with creating new reimbursement strategies to improve quality and decrease costs. Over the past decade, CMMI has tested over 50 new payment models, and in just the last 3 years (2018-2020) CMMI models have reached almost 28 million patients and over half a million health care providers and plans.
Despite these ambitious goals, CMMI reports that “only six out of more than 50 models launched generated statistically significant savings to Medicare and to taxpayers and four of these met the requirements to be expanded in duration and scope.”
In their recently released white paper “Innovation Center Strategy Refresh.” CMMI claims to have learned the following lessons:
- Ensure health equity is embedded in every model
- Streamline the model portfolio and reduce complexity and overlap to help scale what works.
- Tools to support transformation in care delivery can assist providers in assuming financial risk.
- Design of models may not consistently ensure broad provider participation.
- Complexity of financial benchmarks have undermined model effectiveness.
- Models should encourage lasting care delivery transformation.
Some interesting points from the report include:
Medicare FFS beneficiaries will be in an accountable care relationship with providers and will have the opportunity to select who will be responsible for assessing and coordinating their care needs and the cost and quality of their care.
The above seems obvious, but previously, beneficiaries were attributed to physicians typically based on the number of physician visits (often just evaluation and management [E&M] visits). This meant that some patients who would be overseen by a specialist during an acute bout of a disease would be then held responsible for all of a patient’s cost. Further, neither the patient nor the provider would know to which physician the patient would be attributed. While this approach may seem confusing, the benefit was attribution could be done passively; while more active attribution probably makes sense, it is unclear whether patients will actively select providers to manage their care or what will be needed to incentivize patients to do so.
The CMS Innovation Center will address barriers to participation for providers that serve a high proportion of underserved and rural beneficiaries, such as those in Health Professional Shortage Areas (HPSAs) and Medically Underserved Areas (MUAs), and designated provider types such as Federally Qualified Health Centers (FQHCs), rural health clinics (RHCs), and other
safety net providers and create more opportunities for them to join models with supports needed to be successful.
A key question is how CMS will do this. One approach would be to set lower quality or less strict cost evaluations for these types of providers. While doing so would make participation in alternative payment models more attractive, it would also create a two-tiered system with lower quality standards for disadvantaged beneficiaries in HPSA and MUAs who are often treated at FQHCs, HCS and other safety net providers. CMMI have not spelled out explicitly how they plan to accomplish this equity quote. The only concrete action CMMI mentions is collecting data on race, ethnicity and geography to examine health disparities.
Drawing on more diverse beneficiary, caregiver, and patient perspectives will systematically inform development of models that test care delivery changes and innovations that are meaningful and understandable to them….Providers participating in models, particularly total cost of care models, will have access to more payment flexibilities that support accountable care, such as telehealth, remote patient monitoring, and home-based care.
This is clearly a good idea. How to implement more patient-centered care, however, is a challenge. It is good to see that CMS is considering allowing for payment flexibilities around telehealth going forward, but it is not clear why this flexibility would only be extended to providers in total cost of care models; all providers should be able to leverage telehealth to improve patient access and outcomes, not just those in total cost of care models.
CMMI also proposes to lower beneficiary out-of-pocket cost spending, but focuses only on increased use of generic and biosimilars. The Innovation Center also calls for the use of value-based insurance design (VBID). While VBID is sensible, health economic analysis will be needed to determine what treatments qualify as “high-value” and would be subject to low patient cost sharing.
To achieve some of these goals, the CMS Innovation Center aims to go ‘all-in’ on value-based reimbursement and is attempting to expand these payment schemes beyond Medicare. Specifically, they aim to measure their progress as follows:
- All Medicare beneficiaries with Parts A and B and most Medicaid beneficiaries will be in a care relationship with accountability for quality and total cost of care by 2030.
- Where applicable, all new models will make multi-payer alignment available by 2030.
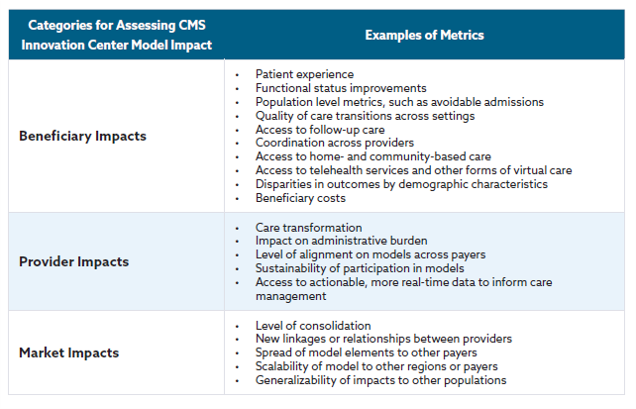
Below is a table describing how CMS will measure success for different stakeholder groups.
There is much more in the white paper and you can read the full document here.