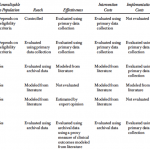
How do you implement a cost effectiveness analysis (CEA) for the implementation of evidence-based practices (EBP)? This is the topic Fortney et al. (2014) address. They review four types of CEAs.
- Trial based CEA. Relies on traditional randomized controlled trials (RCT). Because RCTs are expensive, they are typically run on a small sample of the population of interest.
- Policy CEA. This approach combines the results of a previous RCT to measure benefits but measures cost using the results of an implementation trial. This approach improves the cost estimates for the manner in which the EBP would be implemented but assumes the RCT results are externally valid for the population of interest.
- Budget impact analysis and systems-level CEA. These approaches use decision analytic modeling to estimate how the adoption of an EPB would impact the allocation of treatments to patients in routine care. It estimates the estimates the size of the population reached by the EBP, and the effect of implementation on costs, but clinical outcomes also come from RCTs. Systems-level CEA “predicts both costs and clinical outcomes by having an expert panel estimate the decline in the clinical effectiveness of the intervention when it is delivered as an EBP in routine care.”
- Population Level CEA. This approach measures the ratio of incremental population-level costs and incremental population-level effectiveness relative to the current standard of care.
The authors test how the population-level CEA would work for a rollout of telemedicine-based collaborative care for depression in VA community-based outpatient clinics. The implementation trial focuses on improving adherence to depression medications. The approach used an implementation trial which matched 11 community-based outpatient clinics lacking on-site psychiatrists with 11 other Medical centers based on region, staffing and pre-period patient adherence.
The authors found that the incremental cost of a telemedicine-based collaborative care program for depression was low ($64), but the benefit was also low (0.002 QALY). The incremental cost effectiveness ratio (ICER) was $33,905.92/QALY but this was not statistically different from zero. The authors do not take into account convenience cost to the patient however (i.e., avoiding the need to commute); doing so could improve the ICER from society’s perspective even if not from the VA’s perspective.
Source:
- John C. Fortney, Jeffrey M. Pyne, and James F. Burgess, Jr. Population-Level Cost-Effectiveness of Implementing Evidence-Based Practices into Routine Care. Health Services Research. BESTOF THE 2014 ACADEMYHEALTHANNUAL RESEARCH MEETING. DOI: 10.1111/1475-6773.12247