Last fall, ICER published a white paper titled “Cornerstones of ‘Fair’ Drug Coverage: Appropriate Cost-Sharing and Utilization Management Policies for Pharmaceuticals.” To paraphrase, ICER’s goal is to limit access restrictions (e.g., cost sharing, coverage limitations, prescriber restrictions, step therapy) when a drug is deemed to be cost effective. How will they do this? Their Barriers to Fair Access Assessment Protocol describes the approach. I summarize the key steps below.
- Identify relevant drugs. ICER says that they will start with a list of treatments that were deemed to be cost effective based on ICER reviews conducted between 2015 and 2020. They do not clarify if these are all assessments that started in this time period or ones that were completed in this time period, but I will assume the latter. A key point is that ICER’s definition of cost-effectiveness is when the drug’s incremental cost-effectiveness ratio falls below $150,000 per quality adjusted life year (QALY) or $150,000 per equal value of life years gained (evLYG).
- Updating drug prices. While the drugs may have been cost-effective at launch, price increases could make the drug no longer a good value. To address this possibility, ICER will update how prices change over time. While many drugs prices have increased, so have the rebates paid to PBMs. ICER will used net price estimates from SSR Health to estimate changes in price. ICER will also look at drug price changes from based on a drug’s Wholesale Acquisition Cost (WAC) and the Federal Supply Schedule Service (FSS), particularly if SSR Health does not have available data.
- Final list of drugs. Using this approach, ICER made a list of 28 drug-indication combinations they deemed to be high value.
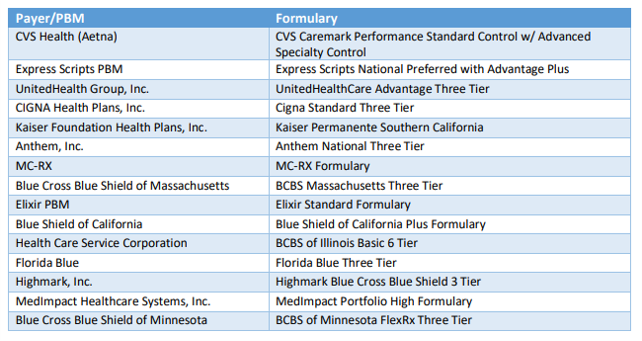
- Review coverage policies for these high-value drugs. ICER will then review the coverage policies for 15 of the largest commercial payers to determine if there are undue access restrictions on these drugs.
What questions will ICER answer as part of this assessment? Originally there were 20 criteria ICER was planning to evaluate, but as part of the assessment to be conducted this year, they will only evaluate 19 of these criteria. The criteria include:
- At least one drug in every class should be covered at the lowest relevant cost-sharing level unless all drugs are priced higher than an established fair value threshold
- If all drugs in a class are priced so that there is not a single drug that represents a fair value as determined through value assessment, it is reasonable for payers to have all drugs on a higher cost-sharing level.
- If all drugs in a class are priced so that they represent a fair value, it remains reasonable for payers to use preferential formulary placement with tiered cost sharing to help achieve lower overall costs.
- Payers should document at least once annually that clinical eligibility criteria are based on high quality, up-to date evidence, with input from clinicians with experience in the same or similar clinical specialty.
- Clinical eligibility criteria should be developed with explicit mechanisms that require payer staff to document that they have: (i) considered limitations of evidence due to systemic under-representation of minority populations; (ii) sought input from clinical experts on whether there are distinctive benefits and harms of treatment that may arise for biological, cultural, or social reasons across different communities; (iii) confirmed that clinical eligibility criteria have not gone beyond reasonable use of clinical trial inclusion/exclusion criteria to interpret or narrow the FDA label language in a way that disadvantages patients with underlying disabilities unrelated to the condition being treated.
- Clinical eligibility criteria that complement the FDA label language may be used to: (i) st standards for diagnosis; and/or (ii) define indeterminate clinical terms in the FDA label (e.g., “moderate-to-severe”) with explicit reference to clinical guidelines or other standards; and/or (iii) triage patients by clinical acuity when the payer explicitly documents that triage is both reasonable and necessary
- Any step-therapy applied is (i) clinically appropriate for all or nearly all patients and does not pose a greater risk of any significant side effect or harm and (ii) if step therapy is applied, patients will have a reasonable chance to meet their clinical goals with first-step therapy.
- Any switch therapy required must (i) be based on the same mechanism of action or presents a comparable risk and side effect profile to the index therapy, (ii) have the same route of administration or the difference in route of administration will create no significant negative impact on patients due to clinical or socio-economic factors, (iii) not require patients to switch to a drug that they have used before at a reasonable dose and duration with inadequate response and/or significant side effects, including earlier use under a different payer.
- Restrictions of coverage to specialty prescribers are reasonable when payers explicitly affirm one or more of the following justifications: (i) accurate diagnosis and prescription require specialist training, with the risk that nonspecialist clinicians would prescribe the medication for patients who may suffer harm or be unlikely to benefit, (ii) determination of the risks and benefits of treatment for individual patients requires specialist training due to potential for serious side effects of therapy, (iii) dosing, monitoring for side effects, and overall care coordination require specialist training to ensure safe and effective use of the medication.
- Requiring that non-specialist clinicians attest they are caring for the patient in consultation with a relevant specialist is a reasonable option when the condition is frequently treated in primary care settings but some elements of dosing, monitoring for side effects, and/or overall coordination of care would benefit from specialist input for many patients.
A lot of these evaluations require some subjectivity. ICER says it will make these determinations by using their in-house research staff to make preliminary judgments and then these judgments will be reviewed by an internist on the ICER staff. Nevertheless, the stringency through which ICER applies these “fair access” criteria will be interesting to see. If a coverage policy is determined not to lead to “fair access” the payers themselves have the ability to provide comment and clarification as well as provide a written comment upon the report’ release. Patient representatives will also be able to weigh in on ICER’s evaluation of whether a policy is fair.