Physician quality is often regarded by researhers as an immutable trait. There are high-quality physicians and low-quality physicians. In most areas where technical skill is required, however, practice makes perfect. A key question is, does ‘practice-makes-perfect’ (aka learning-by-doing) occur for physicians as well?
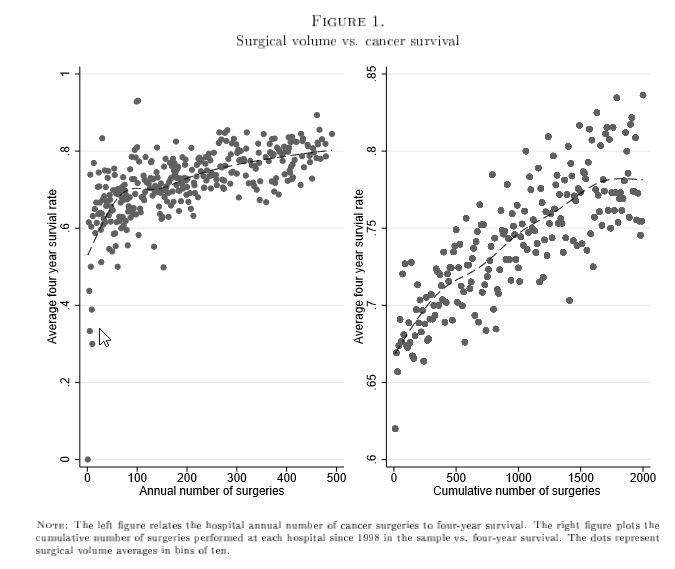
A key challenge when doing this research is knowing the direction of causality. If we observe a high-quality physician with large surgical volumes, it is hard to know whether high-volume lead to better quality or physicians who are higher quality attract more patients. Previous efforts such as Gaynor (2005) and Gowrisankaran et al. (2006) use an instrumental variables approach to answer this question; the former looking at the share of hospitals offering CABG surgery in the surrounding area, the latter measuring patient distance to hospital as instruments. A recent paper by Avdic et al. (2019) looks at learning-by-doing in cancer surgery in Sweden. The figure below shows the descriptive relationship between cancer surgery volume and survival not accounting for endgeneity (from an earlier working paper).
In their paper, Avdic and co-authors use cancer clinic closures as an instrument to identify the causal effect of increased volume, as a closure of a nearby cancer clinic is likely to increase other proximate provider’s cancer surgery volume. The closures were largely in response to a 2000 law that prohibited regional health councils from running deficits, and thus these closures were fairly exogenous in nature. Using this approach, the authors find:
…doubling the per annum number of cancer surgeries in a clinic increases the probability that a patient is alive four years after the surgery with on average 2.9 percentage points…the average elasticity of mortality with respect to operation volume is about -0.12, a sizable effect.
More volume also reduces the number of re-operations and surgical complications. The authors note that there may be decreasing returns from learning by doing as the slow of the volume-survival relationship is steepest at lower volumes.
Further, the learning-by-doing appears to accrue at the physician rather than organizational level. Following an approach outlined by Levitt et al. (2013), the authors find that clinics with lower turnover have a stronger volume-survival relationship compared to clinics with high physician turnover.
In short, for cancer surgeons, practice does make perfect.
In terms of policy recommendations, the authors find that mandating a minimum surgical volume of 70 cases per year would increase the survival rate by 1 percentage point but decrease the number of cancer clinics by 30%. While in a static sense this policy would be welfare improving, I am hesitant to impose minimums since it does not allow more junior staff the ability to practice their craft, and by restricting supply may have adverse outcomes if there are additional wait times. Thus, while I think this is a fantastic piece of academic work, I don’t buy the policy prescription would work in the real-world.
Source:
- Avdic D, Lundborg P, Vikström J. Estimating returns to hospital volume: Evidence from advanced cancer surgery. Journal of health economics. 2019 Jan 1;63:81-99.
1 Comment