Most health technology assessment (HTA) bodies measure treatment value as benefits from reduced patient morbidity and mortality and weigh these health gains against incremental changes in treatment cost. The limitation of this approach, however, is that it may ignore broader societal value. For instance, if patients have improved functional status, caregiver time and cost burden may less; further, patients themselves may be able to go back to work; the public sector may save money from reduced public assistance cost (e.g., people going on disability). This broader value elements were laid out formally by Ladkawalla et al. 2018 which created an ISPOR “value flower” of broader value elements. While these broader value elements may be of academic interest, it is not clear whether the magnitude of these effects is large.
Alzheimer’s disease is one condition that clearly impacts caregiver burden, productivity, the likelihood of going on disability insurance and a variety of other social impacts that may not be directly captured when measuring treatment benefits on mortality and morbidity (often summarized using the quality adjusted life years (QALY) metric). A paper by Prados et al. (2022) aims to quantify the full societal value of new disease modifying treatments for Alzheimer’s disease.
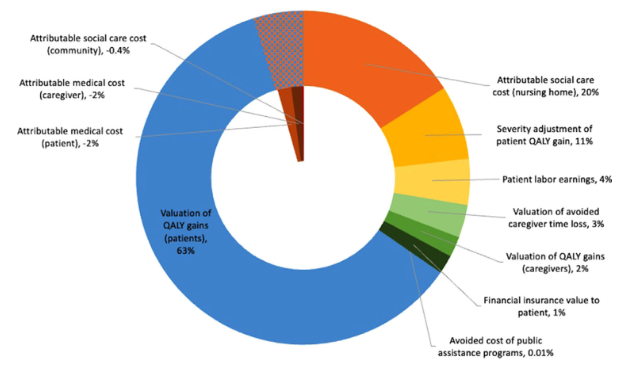
The find that 63% of the treatment value is captured using the standard QALY-based approach. However, the remaining 37% of value is missed due to reduced nursing home costs, productivity, caregiver costs, and avoided public assistance programs. Nursing home and other cost offsets, however, are often included in cost effectiveness evaluation and thus the likely value missed by standard CEA frameworks is likely closer to 20%.
In the figure above, however, the authors mention that this is value specifically related to the patients. Individuals without Alzheimer’s disease may benefit from the treatment as they are at risk of getting Alzheimer’s disease in the future. If they are risk averse, their value of disease modifying therapy may be higher than probability of getting the disease times the QALY-based treatment value. In fact, the authors do find that most of the value of Alzheimer’s treatment’s comes from benefit to those currently without the disease.
We have quantified the value of a disease-modifying AD treatment from a US societal perspective…as a lifetime value for the 2021 cohort of prevalent patients with MCI due to AD disease of $986 billion….We calculate $4.52 trillion in lifetime value of insurance for unafflicted adults (alive in 2021). Thus, overall gross societal value is estimated to be $5.5 trillion, the sum of value accrued to the afflicted and unafflicted cohorts in 2021, as the insurance value to the 2021 unafflicted cohort already captures the value to those who become symptomatic later.
In short, about 82% of the treatment value comes from individuals without Alzheimer’s who are at risk of having the disease in the future. This finding is similar to the Shafrin et al. (2021) paper which found that 89.8% of treatment value for cancer comes from this generous insurance value.